October 12, 2016
Endocrine Disrupting Chemicals and Biomarkers
Introduction
Humans and the environment are exposed to numerous chemicals every day1. Each year, about 2,000 new chemicals are manufactured in the U.S.2. Research findings over the years have shown how some chemicals known as endocrine disrupting chemicals (EDCs) can interact with the endocrine system, disrupt homeostasis, and lead to issues such as obesity and sterility1. As a result, endocrine disrupting chemicals and biomarkers have recently become an important topic in the scientific community. There are many challenges associated with uncovering possible endocrine disrupting effects of chemicals1. Researchers can utilize various hormone biomarkers to understand how EDCs affect the endocrine system and their mechanisms of action in both animal and human models.Overview of the Endocrine System
The endocrine system (ES) consists of specialized organs and glands positioned throughout the body3. Together, these organs and glands work to maintain homeostasis by controlling functions such as growth, development, energy homeostasis, and reproduction3. In order to maintain these functions, endocrine glands and organs synthesize a variety of different chemical messengers called hormones3.Endocrine Disrupting Chemicals
The endocrine system is a well-oiled machine. However, it can be negatively influenced by compounds called endocrine disrupting chemicals1. EDCs are natural or synthetic compounds that can interfere with the endocrine system’s ability to help an organism develop, grow, reproduce, and maintain overall homeostasis1.Exposure to Endocrine Disrupting Chemicals
Exposure to EDCs occurs through many avenues such as consuming contaminated food and/or water, living near chemical plants, working with chemicals, and using consumer goods such as beauty care products4. Furthermore, some EDCs can even be passed from a mother to the fetus during pregnancy and to infants through breast milk5.Mechanisms of Endocrine Disrupting Chemicals
Research over the years has demonstrated how endocrine disrupting chemicals can affect the endocrine system through various modes of action including mimicking and blocking hormones from binding to their receptors6-8. More recently, scientists have discovered evidence that EDCs can modify gene expression without mutating DNA, also known as epigenetic changes7.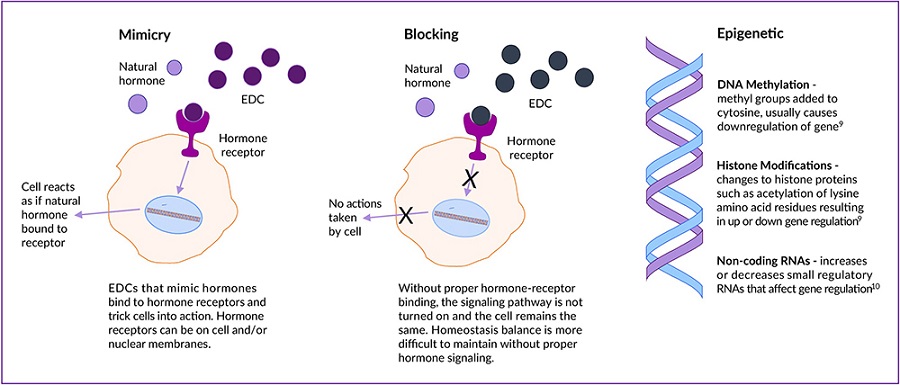
Using Biomarkers to Advance Endocrine Disrupting Chemical Research
There are several challenges associated with specifically testing and regulating EDCs1. These include delayed effects of EDC exposure1, age and developmental stage of EDC exposure1, epigenetic changes7, and the formation of metabolites from the breakdown of EDCs9. Researchers can overcome these challenges by utilizing biomarkers in their investigation of EDCs. Key biomarkers include thyroid hormones, sex steroid hormones, and more recently, biomarkers of diabetes and obesity.Thyroid Hormones (THs)
The primary hormones produced by the thyroid are triiodothyronine (T3) and thyroxine (T4). T3 and T4 exert their effects on several body functions including the cardiovascular, skeletal, central nervous, and reproductive systems, and glucose metabolism. EDCs can interfere with THs through multiple mechanisms such as inhibiting cells from absorbing the iodine needed to make THs or preventing cells from secreting THs10.Estrogens and Progestogens
Estrogens and progestogens are known as “female” sex hormones, but are also produced naturally in males11. Estradiol, estriol, and estrone are all estrogens. Progesterone is the only human progestogen. Proper levels of these hormones are vital for development and reproduction12. Since estrogens are prone to being mimicked, blocked, and having their synthesis disrupted, researchers can utilize biomarkers to analyze each EDC effect1.Androgens
Androgens are considered “male” sex steroid hormones, but they are also found in females. Humans have four main androgens13, with testosterone being the most well-known human androgen. These sex steroid hormones are vital for the proper growth and development of both males and females13-15. Like estrogens and progestogens, androgens can be mimicked, blocked, and have their synthesis interfered with by EDCs1.Adiponectin (ADP)
One biomarker that has become increasingly important in understanding the effects of EDCs on obesity is adiponectin (ADP). ADP is a protein exclusively secreted from adipose (fat) tissue which has been shown to affect multiple areas of the body in different ways16, such as cell proliferation in the pancreas and the regulation of fat lipid metabolism in fat tissue. Research has shown that some endocrine disrupting chemicals can prevent ADP from being released into circulation. Therefore, measuring ADP may be beneficial to researchers studying EDCs and obesity17-19.Conclusion
Hormone balance is necessary to ensure a properly functioning endocrine system. Hormones produced by the thyroid, reproductive tract, and fat tissue work together to maintain homeostasis. Researchers around the world are working to better understand endocrine disrupting chemicals in order to more effectively predict how a chemical may impact health and the environment. Although many challenges in the field have arisen, hormone biomarkers are becoming useful tools for studying endocrine disrupting chemicals.References
- Diamanti-Kandarakis et al. (2009). Endocrine-disrupting chemicals: An Endocrine Society scientific statement. Endocr. Rev., 30(4), 293-342. PMID: 19502515.
- National Toxicology Program. (2016). About NTP. U.S. Department of Health and Human Services.
- Hiller-Sturmhofel & Bartke. (1998). The endocrine system: An overview. Alcohol Health Res World, 22(3), 153-64. PMID: 15706790.
- National Institute of Environmental Health Sciences. (2010). Endocrine Disruptors. U.S. Department of Health and Human Services.
- Stefanidou et al. (2009). Human exposure to endocrine disruptors and breast milk. Endocr. Metab. Immune Disord. Drug Targets, 9(3), 269-76. PMID: 19594415.
- Lee et al. (2013). Molecular Mechanism(s) of endocrine-disrupting chemicals and their potent oestrogenicity in diverse cells and tissues that express oestrogen receptors. J. Cell. Mol., 17(1), 1-11. PMID: 23279634.
- Cruz et al. (2014). Long-term effects of early life exposure to environmental estrogens on ovarian function: Role of epigenetics. J. Neuroendocrinol., 26(9), 613-24. PMID: 25040227.
- Derghal et al. (2016). An emerging role of micro-RNA in the effect of the endocrine disruptors. Front Neurosci., 10, 318. PMID: 27445682.
- Grimm et al. (2015). Metabolism and metabolites of polychlorinated biphenyls (PCBs). Crit. Rev. Toxicol., 45(3), 245–272. PMCID: PMC438329.
- Molehin et al. (2016). Prenatal exposures to multiple thyroid hormone disruptors: Effects on Glucose and Lipid Metabolism. J. Thyroid Res., 2016, 8765049. PMID: 26989557.
- Kimball. (2013). Hormones of the Reproductive System. Kimball’s Biology Pages.
- Sanderson. (2006). The steroid hormone biosynthesis pathway as a target for endocrine-disrupting chemicals. Toxicological Sciences, 94(1), 3–21. PMID: 16807284.
- Tulane University. (2014). The Hormones: Androgens. Endocrine Disruption Tutorial. Tulane University.
- Walters et al. (2007). Androgen actions and the ovary. Biology of Reproduction, 78(3), 380-389. doi: 10.1095/biolreprod.107.064089.
- Meeker & Ferguson. (2014). Urinary phthalate metabolites are associated with decreased serum testosterone in men, women, and children from NHANES 2011–2012. J. Clin. Endocrinol. Metab., 99(11), 4346–4352. PMCID: PMC4223430.
- Nigro et al. (2014). New insight into adiponectin role in obesity and obesity-related diseases. BioMed Research International, 2014. Doi:10.1155/2014/658913.
- Hugo et al. (2008). Bisphenol A at environmentally relevant doses inhibits adiponectin release from human adipose tissue explants and adipocytes. Environ. Health Perspect., 116(12), 1642-1647. DOI:10.1289/ehp.11537.
- Gore et al. (2015). EDC-2: The Endocrine Society’s second scientific statement on endocrine-disrupting chemicals. Endocr. Rev., 36(6), E1-E150. PMID: 26544531.
- Ben-Jonathan et al. (2009). Effects of Bisphenol A on adipokine release from human adipose tissue: Implications for the metabolic syndrome. Mol. Cell Endocrinol., 304(1-2), 49–54. PMCID: PMC2775425.
